A SpO2 sensor is a medical device that measures the oxygen saturation level in your blood (peripheral capillary oxygen saturation) and your pulse rate, typically in a non-invasive way.
Here’s a comprehensive breakdown of what it is, how it works, its uses, and key considerations.
What is SpO2 ?
SpO2 is a percentage that represents the amount of oxygen-saturated hemoglobin relative to the total hemoglobin in your blood.
- Normal Range: For a healthy person at sea level, it’s typically 95–100%.
- Concerning Range: Below 95% can be a sign of hypoxemia (low blood oxygen), and below 90% is often considered clinically significant and requires medical attention.
How Does It Work ? (The Principle)
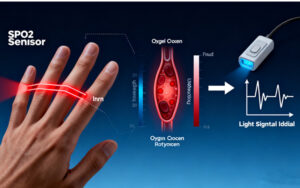
The most common type is the pulse oximeter (the clip-on device for your finger). It works based on photoplethysmography (PPG) and the different light absorption properties of oxygenated and deoxygenated hemoglobin.
1. Two Lights: The sensor emits light from two LEDs (Light-Emitting Diodes) through your skin (usually a fingertip or earlobe):
- Red light (~660 nm)
- Infrared light (~940 nm)
2. Different Absorption:
- Oxygenated hemoglobin (HbO₂) absorbs more infrared light and allows more red light to pass through.
- Deoxygenated hemoglobin(Hb) absorbs more red light and allows more infrared light to pass through.
3. Detection & Calculation: A photodetector on the other side measures how much of each light wavelength is transmitted. The processor calculates the ratio of red to infrared light absorption, which correlates directly with the percentage of oxygenated hemoglobin.
4. Pulsatile Signal: It specifically looks at the pulsating arterial blood (ignoring venous blood and other tissues) to determine the pulse rate and the oxygen saturation in the arteries.
Types of SpO2 Sensors
1. Transmission Pulse Oximeters:
- The most common type (finger clip).
- Light is transmitted through the tissue to a detector on the opposite side.
2. Reflectance Pulse Oximeters:
- Light is emitted and the reflected light from the tissue (e.g., from the forehead, wrist, or chest) is measured.
- Used in wearable devices like smartwatches (Apple Watch, Fitbit) and for sites where transmission is not practical (e.g., fetal monitoring).
Common Applications & Uses
Hospitals & Clinical Settings: Routine monitoring during surgery, in ICUs, emergency rooms, and for patients with respiratory/cardiac conditions.
- Home Use: Managing chronic conditions like COPD, asthma, sleep apnea, and recently for COVID-19 monitoring.
- Sports & Fitness: Wearables for athletes to track performance and recovery.
- Aviation & High-Altitude: Pilots and mountaineers use it to guard against hypoxia.
Key Considerations and Limitations
- Accuracy: Clinical-grade devices are highly accurate (±2%). Consumer devices (wearables, cheap finger clips) can be less accurate, especially at lower saturations.
- Factors That Can Affect Accuracy:
- Poor Perfusion: Low blood pressure, cold hands, shock.
- Motion Artifact: Shaking or movement can cause false readings.
- Nail Polish & Skin Pigmentation: Dark nail polish (especially black, blue, green) and some studies show skin tone can affect accuracy, particularly with reflectance sensors.
- Ambient Light: Bright, flickering light can interfere.
- Carbon Monoxide Poisoning: Pulse oximeters cannot distinguish between carboxyhemoglobin (CO-bound) and oxyhemoglobin, giving falsely high SpO₂ readings. This requires a co-oximeter (used in hospitals).
- Irregular Heart Rhythms: Can make it difficult to get a stable reading.
What It Does NOT Measure:
- It does not measure the actual oxygen level in your blood (PaO₂ from an arterial blood gas test).
- It does not measure ventilation (how well you’re removing CO₂).
- It is not a complete measure of respiratory sufficiency.
Recent Advances & The Future
- Smartphone Integration: Apps using phone cameras/flashlights (though less accurate and not for medical diagnosis).
- Advanced Wearables: Continuous, 24/7 monitoring in smartwatches and rings (e.g., Oura Ring, Whoop).
- Multi-Parameter Monitoring: Combined with ECG, temperature, and blood pressure in single devices.
In Summary
A SpO2 sensor is a vital, non-invasive tool for instant feedback on blood oxygen levels and heart rate. While incredibly useful for screening and trend monitoring, it’s important to understand its limitations and not rely solely on it for diagnosing serious medical conditions—always consult a healthcare professional for interpretation and diagnosis, especially if you have symptoms like shortness of breath.
